Submissions from Readers
Motivation
by Marilyn
(Prescott AZ)
Question: My husband had a stroke 2 years ago. It affected his right side. He walks with a cane and a little without one but can not use his right hand. He is left handed so he can do a lot of things. How can I keep him motivated?
Answer: Here are some tips to help keep him motivated:
1. Have him participate in activities that he enjoys. If he had a favorite hobby before that is now difficult, try to adapt the hobby so that he can participate. You can also help him find new hobbies.
2. If applicable, involve younger children and grandchildren to make activities more fun and motivating to him.
3. Do activities with peers. Continue to be active socially and have friends help you keep him motivated.
4. Keep a chart of exercises and progress.
5. Set goals and work on achieving each goal. Goals make one's action have a clear direction. If a goal ends up being too difficult then choose an easier goal.
6. Celebrate when a goal is achieved (e.g go to a favorite restaurant, go on a trip, make a favorite meal, get a massage, etc.)
7. Don't nag and try to keep a positive attitude and outlook.
8. Have him read positive mental attitude or encouraging books (or listen to them online together or via audio tapes together).
9. If you use certain equipment for therapy, keep it easily accessible and visible (out of sight=out of mind and will lead to not following through with exercises)
10. Have him exercise with a partner that will hold him accountable for exercising (a friend or maybe another stroke survivor).
11. Hire a personal trainer that has experience in working with stroke patients.
12. Vary his routine to prevent boredom.
13. Make sure he gets enough rest and does not get over fatigued.
14. If you tend to help him too much, stand back and make yourself less available so that he must become more independent in doing for himself.
15. Continue to treat him as your equal. Don't coddle or treat him as a child. This can be demeaning to a person who has had a stroke.
There are many people that live enjoyable, fulfilling lives that have disabilities. Attitude plays a big part in how a person responds to a disability. This is true from the perspective of a caregiver as well.
Comments for Motivation
|
||
|
||
|
||
|
||
denial of limitations
Question: My husband had a stroke 6 months ago and has never accepted his limitations. He tells doctors he can perform a cardio-stress test on a treadmill when he cannot walk more than 100 feet, and that with 2 crutches! He is sure he can drive, although he shows poor coordination and sudden fatigue. He refuses any assistance with doors, chairs, etc. and asks "Why are people treating me like an invalid?" He wants to travel although he cannot lift a suitcase. He will not go in the "handicapped" line anywhere. Although he gets exhausted and must sit down to rest after a few paces, he will not use a wheelchair. We cannot go to museums or zoos because of that. He holds on to furniture in the house because he will not use canes. He will not wear support hose because he "does not need them". He will not wear a napkin or bib because he does not realize he dribbles whenever he eats, even when he sees it on his shirt. This is driving me nuts. Even when the consequences are staring him in the face, he will deny it. What's to be done? He has never moved out of this "phase".
Answer: This isn't necessarily a "phase" but may be likely due to the part of the brain that was affected. You do not mention what part or side of the brain was affected, but he demonstrates many of the symptoms of a right brain CVA with left side extremity weakness. Some of the characteristics of R brain strokes are impulsiveness, trying to do things without help which may be dangerous, showing little awareness of problems from stroke, restlessness, agitation, and denial of disability. You may benefit from asking the MD what areas of the brain were affected and then researching the effects of damage to those areas. I suspect your husband has had damage that is causing these behaviors. You can look online regarding ways to deal with patients that have had a R brain CVA (or with damages to other areas). This may help you learn better techniques in dealing with him. You could also have him work with a speech language pathologist, cognitive therapist, or a neuro-psychologist.
Post stroke father refers to left arm as child
Question: My father is 3 yrs post stroke with left side paralysis. He refers to his affected arm as her/him. He asks "child" questions and talks to arm throughout day. Md and I have explained to him that feeling in his arm is result of stroke. He will accept answer but in next breath refers back to his "child". I just want to know how to handle this. Do I try to reorient him or go along with his delusion?
Answer: Since he has been doing this for three years, I personally wouldn't bother in correcting him. You don't have to go along with it (meaning you can still call it his arm though he calls it his child), but I wouldn't go out of your way to explain things over and over again as he doesn't seem to be taking it in.
Why NO TPA!!
by Nana Rose
(Houston)
Question: In the past I would see ads on stroke and TPA here in Houston. I memorized these ads and shared with my kids and other family members. In June, something happened to me. 911 was called at 10:00PM at night. I went to bed at 7:00PM and awoke for bathroom break at 8:30PM, talked with hubby, went back to bed and awoke again at 10:00PM for bathroom break but could not function my eyes. I was petrified. Hubby dialed 911. They put me on a moving office chair and took me to the ambulance in the driveway. There I sat for 30 minutes while they talked and made calls. Hubby wanted me at our doctor's hospital in the Med Center but they said they had to take me somewhere else. From there they lifeflighted me to another hospital in the Med center. CT scan showed a clot in the Cerebellum area.
I did not have any TPA although hubby asked for it. I do not remember much. The helicoptor ride, yes. I do remember the 911 lady cutting my jammies off of me with scissors. Now, 6 months later, I am not well. I feel had I was given the TPA shot (well within the time zone) I would be so much better. What prohibits them from not using TPA when one is in the safe time allowed. I had 4 weeks in a rehab place and 6 weeks in home health care PT. I may be 25% better but no more. I am scared in fear that this will happen again and no TPA. Do they still use TPA? We were told if I feel I am having another stroke to get to the nearest hospital ASAP. WHY? if they do not use TPA?
We know we will have to drive ourselves if we want to go to our own hospital where our doctors work, i.e. Cardiologist and neurologist. I also need to know if insurance plays a part in treatment. I am a Medicare patient and Policy permits me to go anywhere. I am diagnosed with a moderate insult of the cerebellum. My balance is way off as well as co-ordination. Does it and can it improve months later? Thank You. Nana Mary
Answer There are several contraindications to using TPA. The best way for you to find the answer is to present your question to the treating physician or facility so they can elaborate on why they did not choose TPA for you. You can visit this link that lists some of the contraindications to using TPA: https://icahn.org/wp-content/uploads/2018/10/stroke_inclusion_exclusion_stroke_.pdf.
If you are concerned about having a future stroke and the care you may receive, you can research what the closest facility is to you that is accredited in stroke treatment and asked to be taken to that facility. Obviously, some individuals do not live close to such facilities, but doing research ahead of time will at least help you know your best option. If you live near Houston, there should be options.
As far as your question regarding recovery, I would not be able to predict how much you can improve, but yes it is possible to make improvement. If you do an online search for cerebellar stroke recovery, several blogs and forums pull up from stroke patients who detail their experiences. I believe this would be encouraging to you and allow you to see what others have achieved.
Hopefully you are working with an experienced therapist or have worked with one and have a home exercise program to continue. Since you have Medicare benefits, I would see if there is an outpatient facility near you that offers therapy. An outpatient facility will provide you more equipment to work with and will probably be more intense than home health. You could also look into working with an exercise professional who is experienced in working with stroke patients once you exhaust your therapy benefits.
I actually just came across a facility online today that is in Katy, Texas called Medical Fitness Pros. They have personal trainers and other professionals who have been trained and have experience in working with clients who have medical conditions. There are other facilities like this as well. These are not a substitute for physical or occupational therapy, but if you have exhausted your therapy benefits and would like to continue to exercise and work on balance, then places like these are an option but are not covered by insurance.
One thing to consider with your Medicare benefits for therapy is that they have caps and thresholds, and you are usually responsible for 20% of the copay for outpatient services. To find out more about what Medicare covers, visit https://www.medicare.gov/coverage.
Comments for Why NO TPA!!
|
||
|
||
Mom lives over seas - 2 strokes within 1 year.
by Lucia Aleixo
(Eastchester, NY)
Question: My mother is 79 years old, diagnosed by-polar over 30 years ago and lives in Portugal with my father. She has a healthy diet, has lost weight but is not active. She had a TIA last February and 11 months later her second TIA stroke. First stroke affected her speech and the second stroke affected her left arm with some short term memory loss and slow speech. Both times the stroke affected her mood (became more depressed). Since it is difficult for me to communicate with the doctors over seas, what should I be asking them to do for her and give me in order to ensure that my mother is getting the appropriate x-rays, tests, re-habilitation and the best care possible? In addition when she returns home should she try mild exercise?
Any advice you can provide is greatly appreciated. I'm very worried for my mother's health and well being.
Lucia Aleixo
Answer: After having a stroke, it is important to follow up with a neurologist and also to see one's family physician on a regular basis to be monitored. Normally physicians will monitor things like blood pressure and blood work. After a patient has stabilized from a stroke and has their M.D.'s okay, it is usually not a problem to do exercise (assuming they don't have other medical complications that would limit their ability to exercise). If depression is an issue, it may be a good idea to do a consult with a neuro-psychologist or neuro-psychiatrist who specialize in working with emotional and personality disorders related to neurological problems.
New Movement
by Susan Saxton
(Illinois )
Question: My sister now 58 had a stroke 15 months ago she could not move her left side of her body. She was in therapy for only 3 weeks because that is all Medicare/Medicaid would pay for. She has been in a nursing home since. 2 Weeks ago she starting moving her left foot slightly. This past Saturday the nursing home dropped her and she broke her Femur bone on her left side. The Nursing Home did Xrays 3 hours later and called her doctor and the doctor said get her to the hospital the Doctor gave these instructions at 2am, she did not make it to the ER until 6am. We asked the Nursing home what happened. They blamed it on my sister not holding on to the nurses neck and they said they felt her slipping and "laid" her on the floor. Needless to say we are filing a lawsuit. But now after the surgery last night, she was moving her foot a lot. You say move your foot Sissy and she was able to bounce it around. If we get a settlement I would like to put her in a rehab facility for as long as possible. Am I being too hopeful? Do you think there is a possibility of her getting any mobility back on her left side? (BTW the doctors did not expect her to live this long after the stroke) so she is a fighter.
Answer: Three weeks is a very short time to have therapy, so your sister may have achieved better recovery if she had been given more time. I don't know what your sister's experience was in the nursing home. If she was left in bed a lot or had very little stimulation, then she may be able to make some very good gains if now given the opportunity to do more. This doesn't necessarily mean she will regain movement, but if no one was working on moving with her then you don't really know her capabilities. Also, now that she has fallen, she has a new diagnoses which will allow her to have more therapy which I would definitely get her involved in. Once she gets back into therapy, you'll be able to determine how much she is moving and what she can do.
Soooo worried
by Nikki
(Trinidad)
Question My mom had a stroke that affects her right side two weeks ago today and she's not staying put she keeps getting up and trying to walk around and falls , we can't leave her alone for a second she tries to get up ,she's sleeping for short periods at a time and these last two days I realize she's not responding like before. She was talking quite normal but now she refused to open her mouth to say anything and she doesn't seem to be aware of anything since yesterday,could it be the lack of rest is causing her to worsen?
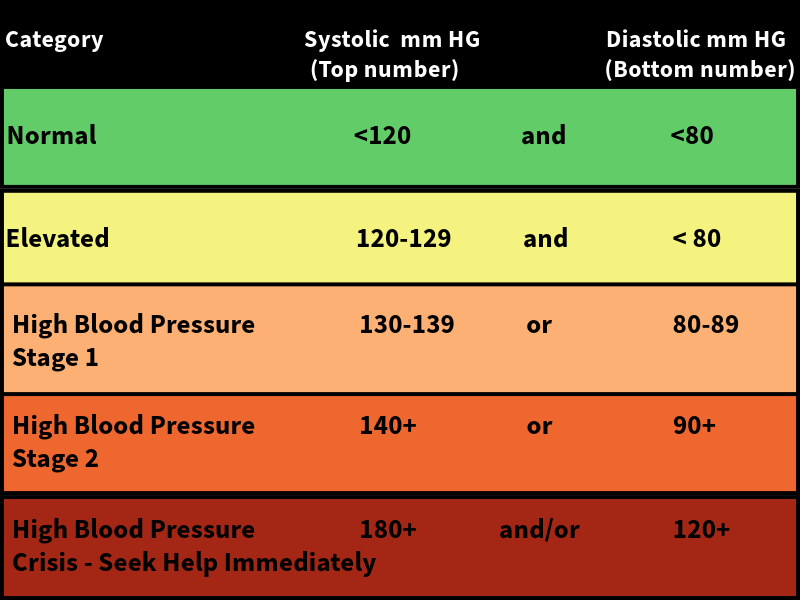
Answer: Lack of rest or being tired can cause symptoms of stroke to be magnified. For example, some stroke patients at the end of the day may present with more slurred speech, more impaired cognition, or more visibly noticeable physical effects. However, worsening of symptoms could also signify something more severe such as a TIA, a new stroke, or conversion of the current stroke, so if her symptoms seem different or magnified such as you have described, then I would take her to the hospital emergency room. It's also helpful to monitor heart rate and blood pressure which might also give you clues about her condition. Obviously high blood pressure or irregular heartbeat would be a concern if it was present.
MOM'S RECOVERY IS INCONSISTENT IS THAT NORMAL?
by Damon .M
(Long beach, ca)
Question: Hello, my mom is 73 years old and this is her second stroke. Her first stroke was in 2011. The doctor called it a speech stroke. h]Her mobility was not affected but her focus, cognition, memory, thinking and comprehension were affected. This 2015 stroke first affected her right leg only. She had minor weakness for the first week and no right arm problem at first, but after the first week in the hospital her right arm got really weak. After her blood pressure was stable she was transferred to the rehab center. When she was there, her balance was slightly off but she sat up on her own for about 30 mins. She needed about 50% assistance standing and walking. She would have done better but her focus was not there when it came to rehab instruction or commands. Also, she became apathetic and slightly depressed and didn't want to participate willfully. So the insurance dropped her down from acute rehab to SNF. When she was transferred to SNF, her progress went down for the first week she was there, and I got scared. I thought it was another stroke but I couldn't tell if was. The week after she started to progress again but slower than she was at the acute rehab center. It has been one month and her balance is improving, her standing is 30%, she has good days and bad. Her left arm and leg is really strong. Doctors have told me she will walk again since she had a minor stroke, but give it 3 to 9 months. Right now I can't see that. Is this normal for stroke patients to do good for two weeks and don't do that good the next two weeks?
Answer: It is not unusual to have fluctuations in rehab performance after stroke. Many factors can contribute to this including fatigue, lack of sleep, dehydration, becoming accustom to a new environment, brain changes and healing, effects of medicine, etc. Also, when an individual changes from one facility to another, the new staff have to get to know the patient. They may be more cautious and not be aware of the patient's capabilities so it may seem that the patient has declined, but in reality it could just be the new caregivers doing less complicated tasks until they know how well the patient can balance and transfer. Give it time, your mother should continue to improve, and there will be day to day fluctuations in her performance. If you noticeable a considerable change such as new paralysis or a significant change in mental status, bring it to the attention of the doctor as this could be a new stroke or other medical problem.
Help for my son after two massive strokes age 40
by Suzen Middleton
(Byron Georgia USA)
Question: Where can I find shoes for my son that his right side is paralyzed? Where can I find help for him for his memory loss, reading, writing and loss of use of his right arm and leg? He is disabled on SSI.
Answer: There are some online stores that sell clothing and shoes that are easier to use for those that have a handicap or that have experienced a stroke. You might be able to find a shoe that works at http://www.silverts.com/show.php/list/men/footwear
As far as help with memory/reading and his arm/leg, I would get orders from a doctor for speech, physical, and occupational therapy. They have home health or outpatient therapy centers available. If for some reason, therapy is not covered by insurance or he has exhausted his insurance, I would see what programs his state offers. You are writing from Georgia. Here is a website that explains programs offered in Georgia:
https://www.olmsteadrights.org/self-helptools/advocacy-resources/item.6532-Georgia_Disability_Resources_and_Advocacy_Organizations.
I would pay close attention to the information under Physical Disabilities Services which can be found toward the bottom half of the page.
Lifting a patient with left side neglect
by Regina
(Melbourne, Florida)
Question: My mother and 86 year old retired nurse midwife had a right hemisphere stroke and is now in rehab. I have seen numerous nurses and CNA care for her and lift her incorrectly.
Not only was her left side affected, when she fell she fractured her first and second rib and sternum on her right side.
I met with Risk Management at the facility asking if they can do anything about the poor communication with the staff and change of shift information that is supposedly carried on from one shift to another.
They moved my mother closer to the nurses station in a room with a window view and no room mate. They continue to move her incorrectly. I don't want to create animosity between staff that care for her nor do I want my mother to bear the brunt of my concerns while I am not there to watch.
I asked an RN coming on the next shift if she knew what happened to my mother because I noticed her moving her incorrectly and my mother experiencing pain in the right side that had the fractures where the RN was pressing on her while lifting her.
RN reply: I don't know
Of course I was in horror and the RN was embarrassed per Risk Management.
The CNA's the same. One goes on break another covers the shift and knows nothing of my mothers condition or the terminology.
WHAT DO WE DO?????
Answer: In facilities where I work, we have a white board where precautions and information about how to transfer is posted. I would suggest you get your own white board or just a piece of paper with instructions in large letters, and place it on the wall above her bed so that all staff can see it when they come in to move your mom. If they have a problem with HIPAA or privacy, have your mom sign something saying she wants the information posted for her care.
Losing Driving Privileges
by Gre
(Albuquerque,NM)
Question:How do I tell a very independent brother that he can't drive anymore or fly his plane anymore due to stroke and cognitive changes in his brain.
Answer: Driving and flying a plane are a matter of public safety. I would just tell him that he at least has to check with the regulating agencies to see if he is okay to drive and/or fly. If he didn't listen then I would report his condition to the appropriate authorities who could evaluate him to see if his license needs to be revoked. I would check with your state's department of motor vehicles and whoever is over licenses for pilots which I assume is the FAA. I know you want to consider your brother's feelings, but this is a matter of human lives which is more important than feelings. There are regulations for driving and flying after a medical event, and if he drives or flies and has any wrecks or incidents, he would be in trouble. He can always take a driving exam again to see if he is safe driving. He also should report to the FAA his change in condition and find out their rules as far as flying.
What should I be doing around the house for my paralyzed mother
by Hayley Ann Klein
Question: I'm 13 years old and my mom Debbie had 2 strokes when I was 8 months old. I have been doing everything a mother should be doing ever since I can remember. I do the dishes, laundry, cook,clean, dress her, bath her. But I got a text from my mom's friend saying that I do to much for my mom and that she needs to go to a nursing home, and that I could live with them. But I don't want to live with them, and I don't think she should be the one deciding if my mom needs to go into a nursing home at the age 45. So basically my question is,"Am I doing to much for my mom? And should she be in a nursing home now?"
Answer: If you personally feel comfortable, don't mind helping your mom, and are able to help your mom, then there is no reason why she should go to a nursing home. If on the other hand, you are overwhelmed, then I would talk to other older family members and see if you can get some help from others or outside resources. You may not have the same lifestyle as other 13 year olds, but that is okay. It just means you will most likely be more mature and able to deal with what life throws your way. Many teenagers back in the 19th century did these activities and more, so there's no doubt you are capable.
I personally think it is noble and loving what you are doing for your mother. Many people don't exhibit that kind of compassion. If you are comfortable with what you are doing, then don't worry about what others think and just keep doing what you're doing. If on the other hand, you are overwhelmed then you need to discuss it with your mom or other close relative.
As with any caregiver, you want to make sure you still have time and fun for yourself so that is where it's important to have other friends and family help. If your mom is able to discuss these issues with you, I would talk to her about it if you are feeling overwhelmed.
Mini Stroke in the elderly.
by julia m harrison
(northwich cheshire UK)
Question: My Mum-in-law had a mini stroke 5 weeks ago, She is recovering slowly and her speech is coming back. She is 87yrs of age. She says she feels tired more but has trouble sleeping. I saw something on social media that when someone of this age has any kind of stroke they will probably have another one with in a short time and it could shorten there lives. How true is this. ? Do some people survive with the right help. She is well in other ways. Eating etc.
Answer: It is true that someone that has a TIA has an increased chance of having a stroke, but there are those that have TIAs that do not go on to have a stroke. I would just have her follow the advice of her doctors (for example if they recommend medication for high blood pressure or for blood clotting issues). I definitely wouldn't worry about the unknown. My grandfather had a stroke at age 80 and then went on to live to 98 without any further known strokes.
Family Discourages Walking
Question: My mother had a stroke the end of June and since then has had several weeks of physical therapy. She is able to walk with assistance and I had been doing this with her every evening. Walking to bathroom, kitchen, bedroom. However, a sister who lives with her insists a nurse from her insurance company, as well as her in home physical therapist, says that I should not walk her. I am told the PT only walks her a few feet each time on his twice weekly visits. She was in the habit of walking more each evening with me, but now family lifts and wheels her around in wheelchair and gets hostile if I try to walk her, as we had been doing. Why would a PT or nurse suggest that my mother not walk, as she is capable of walking up to 150 feet? I am worried that this will adversely affect her long term recovery. My mother is happy to let them wheel her around and is now taking very few, if any steps. I am not there when the PT comes, so am unsure if she's even walking the few feet twice a week.
Answer: I would schedule to be there one time when the therapist is there, and show them what your mother is capable of doing. Then you can discuss a walking plan with them that is more appropriate and get it in writing to show your other relatives.
Comments for Family Discourages Walking
|
||
|
||
Friend of stroke victim with Thalamic Pain Syndrome
Question: I have a friend who had two strokes about 12 yrs ago and has suffered with horrible migraine type pain that he says is 24/7 365 days a year at the level of 7-10 on the pain scale. He does not remember before his strokes, and he loses a lot of memory day to day. It just slips away. I sometimes don't understand why he even remembers me at all. Our relationship when we met was intense and we talked many hours a day as he can't work and I was only working part time. But slowly he has been falling away from me and says he can't remember most of what we have done together and just recently sort of admitted he doesn't remember how he feels about me although he still talks to me almost every day and calls me pet names that he has had for me. I am having a hard time dealing with this. I want to be very helpful and caring and understanding but he is falling away from me and I have put a lot of effort into this relationship and he is forgetting it. It feels like he is being a jerk ... could he be using his illness to pull away from me or is he really losing his memory of me and doesn't remember how close we have been? I feel so bad for him, his life is mostly sleeping because he is on so many meds and can't function because of the pain. I was trying to be a helpful person in his life, I love this man, but I am heartbroken that it has come to this and wonder if I should completely stop expecting him to live up to the standards of what I deem to be appropriate behavior for keeping friendships and living up to what you have said and have acted in the past... obviously this is quite complicated but I don't want to just walk away because I care so much, but this breaks my heart and I feel like I have been taken for granted.
Answer: If it has been 12 years since his stroke, then your friend's condition is most likely not a symptom of his original stroke. It's more likely due to changes in his brain over time. He may have some dementia setting in or he could have been having ischemic events that have affected his memory over time. Based on the symptoms you describe, I doubt he is trying to use his illness as an excuse. I think he is slowly losing memory. This can be tragic for family and friends especially when a loved one begins to forget relationships and even people. I don't know who else is in his life that can help, but it sounds like he may need evaluation by a physician and that he should be monitored closely to make sure he is safe at home. If he is beginning to forget relationships and people, his memory in other areas is most likely affected which can be dangerous when living alone (e.g. leaving on ovens or hot appliances, forgetting keys or directions to home, forgetting to pay bills, etc.)
massive stroke with bone removed to relieve pressure
Question My husband suffer a massive stroke and had his bone removed from the right side. He had a tracheotomy. He can speak words with the speaking valve and its low. He is sleeping a lot until he can't get through therapy without falling asleep. I asked him is he sleeping at night. He said No its the noise. The Rehab place is pretty quite at night. I spoke to the MD about but she just shunned me off.
It has been a month since the stroke and now he is in intense Rehab 3 hours a day for six days. He can remember things and write things down its a little shaky. He doesn't have any movement on the left side at all. He has a feeding tube and still learning to swallow. His vision is off. I know he sees a little colors. He say he sees me. I really concerned about how things are going. He has to have surgery again to place bone back.
Will he be able to survive since he already had a massive stroke? This is the second one. The first one 4 yrs 2013 now 2017. I am scared of all of this and know my husband would not want to live this way. I have to go back to work soon and night school. I am afraid that I want get a chance to visit him daily. I feel guilty. What things will he be able to do and how long it will take. I pray that he don't have to go into a nursing home.
Please let me know how to cope with a sudden change in our lives. Thank you for your help!!
Answer: I am sorry that your husband and you are going through all of this. I know many caregivers are fearful and have many questions. I cannot make any predictions regarding recovery. It's best to talk to his neurologist about the prognosis. Probably the best advice I can give you is to join a support group. Other caregivers can help answer your questions and provide support as well as make suggestions for helpful resources. Sometimes people improve greatly after stroke. Many times people are left with long term impairments, but they can learn to adjust and still live fulfilling lives. Be there for your husband for encouragement and support. When you go to school and work, you are providing means for your family to make it and for him to get the healthcare he needs so try not to feel guilty. He will go through different phases of recovery and will deal with lots of negative feelings and emotions (as will you). Don't rely solely on yourselves. Reach out to friends, family and other stroke survivors and caregivers for support to get you through this.
Rehab
by Laurie H
(Minot, ND)
Question: My husband who is 62 suffered a right MCA stroke - he has been an active science teacher up until November 20, 2015. We have been fighting with Blue Cross Blue Shield about covering rehab for him. He is making slow progress. He has progressed from being unable to sit to sitting unsupported as well as from using a Hoyer lift to being able to transfer by myself. I wonder if there are some avenues for rehab that we are not aware of.
I have taken him home from a nursing care/rehab facility. He is unable to walk, and has some movement in his left leg, but nothing in his arm. He has sensation and feels pain in both the arm and leg. I will not have him living in a nursing home and have taken him home. BCBS has denied coverage in an inpatient acute rehab. He has hopes of returning to teaching this fall. Do you have any advice. We live in Minot ND. with limited access to stroke rehab. We would be interested in some trials if he would qualify also. We feel like we have been given up on and sentenced to life in a nursing home!!!
Answer: I know you said that inpatient was ruled out by insurance, but have you checked into both home health and outpatient therapy options? I would start by looking into those if you haven't already. Outpatient would be preferable due to access to more equipment, but I know that is not always an option for some people. If insurance resources are limited, you might hire a therapist to come out for a few visits (you can do private pay if insurance won't cover it) and have the therapist set up an exercise program that you can follow with your husband. Then periodically, you can have the therapist come back and upgrade the program as needed (this assumes you have time to work with your husband yourself). This option would allow a therapist to at least design a home program for you and get you started if you can't pay or insurance won't pay for regular therapy visits.
There is also a lot of information online including this website that gives you stroke rehab and exercise information that you can use at home on your own. I would also check with your state and see if there are any programs available. Many states have programs for persons with disabilities that want to return to work including providing therapy and making adaptations so one can return to work. Here's a link to the ND website for this:
https://www.hhs.nd.gov/vr
Good Luck!
Best place to bring my sister after a stroke
by Thien
(Clearwater FL)
Question: My sister had a stroke. She cannot take care of herself. She needs 24/7 supervision and someone to bathe, clean, help her with bathroom issues, cook and pretty much everything. What are my alternatives? My niece wants to bring her to her house. She has a husband, and 2 kids and they fight all the times.
Answer: I don't know if your sister's stroke is recent or older, but if it is recent, I would first make sure she goes to a rehabilitation facility to see how much she can improve. If she is still dependent, then it may be best to look into a skilled nursing facility. Many stroke victims do go home with family as well. Some families will provide more attentive care than may be received at a skilled nursing facility, but it can be very stressful to be a caregiver especially if there are already other responsibilities such as taking care of children or working or if there are strained relationships such as those that can occur between spouses.
If your niece wants to take what I presume is her mother home, it is important for her to know the responsibility and sacrifice involved and that it will likely cause even more strain on her marriage. At the very least, I would have home health assist as long as possible if she decides to take her mother home with her. It definitely can be done, but it's very important for caregivers to know what the responsibility entails, what sacrifices will have to be made, and to consider what is best for the patient and caregiver. If your niece does decide to take your sister home with her, I would offer as much support as you can (ask family to help give her breaks, buy groceries, offer childcare, etc.) to lessen the burden. I would also talk to her about being open to trying other options if it doesn't appear to be working out or if it causes too much strain on her relationship with her spouse. If she has the financial means, it would probably be best to have a hired caregiver help with her mother at home.
If on the other hand, your niece decides to look into a skilled nursing facility. I would tour various facilities, look at reviews/complaints, make sure they are experienced with stroke patients, talk to residents and thoroughly investigate before placement.
Helping
by Thrtesa
(Rogers Arkansas usa)
Question: My husband had several mini strokes only problem is he has short term memory loss but he feels he doesn’t have to help do anything around the house he’s capable of doing things but just doesn’t.
Answer: Having a TIA or stroke does not mean that you have to stop doing activities. Of course some people will have severe impairment and may not be able to help due to physical disabilities, but a stroke or TIA in itself doesn't mean you need to stop doing things you did before. In fact, it is recommended that people who have had a stroke get a certain amount of cardiovascular exercise and strengthening just like other individuals. Besides a physical limitation, there may be certain rare cases where activity has to be limited due to medical problems, but the MD should let you know if that is the case. Maybe you can go with your husband on his next doctor visit and have the doctor let him know it's okay to do housework, so he can't use the TIA as an excuse.
Caregiver Question
by June Brown
(Dallas, Texas USA)
Question: My boyfriend had a stroke and is coming up on his one-year anniversary of the stroke. He is doing well with the exception of his left hand, which he is working on with physical therapy. As his girlfriend and caregiver, how do I "handle" this upcoming occasion?
Answer: I think this really depends on the individual. For some, this may be a really traumatic day, some embrace the day and show great determination, and for others it may hold very little significance (probably also depends on severity of stroke). This is one of those questions where I may ask around on stroke forums and see what other stroke survivors say. My inclination would be to accentuate the positive in the sense of look how far you've come and here's to continued recovery and emphasize that you are there for him. Again, it totally depends on the individual.
Difficult patient
by Ah Cheng
(Johor, Malaysia)
Question: I'm currently handling a patient who is very passive and non-compliant to exercises prescribed. Even on my supervision, repeated verbal and visual clues, patient showed little or no effort as if giving up. Caregiver reported that he is fully dependent and situation is even tougher with family members (which he will at least listen to therapist's command a bit)
Prolonged time, condition gradually becomes worse due to immobility and lead to secondary complications such as DVT, extremities swelling and severe muscle atrophy.
Any suggestions on what I can do? I feel sad and helpless seeing patient like this.
Answer: Stroke can cause changes in the brain that effect motivation. I would suggest talking to the doctor and see if there are any medications that can help with decreasing apathy and improving motivation. I would also suggest bringing in a neuro psychologist or neuro psychiatrist to visit with the patient, and they may have medication recommendations as well. Another way to address the problem is to try and identify anything that motivates the patient and incorporate that into therapy. If you can find something that really interests the patient, the patient will be more likely to participate. Make sure the patient is setting the goal, and that you are addressing the patient's needs. As therapists, we often focus on what we think needs to be addressed, but if the patient isn't interested, then it won't work. You have to know what interests the patient.
Lies of Care
by Jay More
(Michigan )
Question Mom had a stroke in 2019. Since then she let the oldest child take over, treats the other children mean, and will not go to her neurologist. It has been three years now. She will not go to the doctor, will not do physical therapy, finds ways to run sitters off, just want her children to do round the clock care for her. Before this stroke she had one when we were young but never followed up with that one. She is retired and hasn't gone to a doctor for 40 years. She is 89 now and still will not go, but we children are in our early sixties and can not pull on her like she wants. She's at risk for falling, so she sit in her manual wheelchair for 14 hours a day. She has gained a massive amount of weight, refuses to use all the help aides to help her around her home, and she even has a brand new electric wheelchair but won't use it. She is controlling, fussy, accusing certain child of stealing her stuff. The oldest child and another have made Mom's stroke about them to make it easier for them to help, but two other children the three hold to the grind without even asking how they are. Now, these two children are out hurting and in physical therapy to gain strength back. Me, I'm out of caring because of the mistreatment, disrespect, and lies/ cover up. What do the two do leave or stay?
Answer:: Unfortunately, these are complex questions that only each child can determine for themselves. Caregiving is very difficult, stroke patients as well as aging parents whose mental status has declined can often be demanding and unrealistic in their expectations though many don't even realize what they are doing. It's important for caregivers to take care of themselves as much as possible or they will get burnt out. If there are multiple caregivers that can help, that would be beneficial so the burden doesn't fall on just one person, but obviously if there is conflict between caregivers, this can become problematic. If caregivers are able to work together and come up with a care schedule, then I would recommend that, but only each child can decide if they want to be involved in that process or act as a caregiver as each person has their own set of life demands and physical/emotional issues.
Only Plays Internet Games and Nothing Else Three Years Post Stroke
by Jazzbea
(Chicago, IL)
Question: I know playing games for up to 8 hours on the internet is not healthy for anyone. Does anyone know how sitting all day long playing games on an iPad impacts a stroke survivor?
My nephew will not participate in anything that will help him. Is this depression? He had his stroke over 3 years ago and was doing better when he first got out of a 57-day stay at inpatient rehab. Although he says he wants to get to the point of being more independent, he won't do the work. He gets angry and has outbursts when he is nudged to do his exercises. He then refuses to eat or drink anything and just lays in bed doing nothing. It's a bit of a challenge.
Answer Research has linked sitting for long periods with several health concerns. They include obesity, increased blood pressure, high blood sugar, excess body fat around the waist, and unhealthy cholesterol levels. All of these put increase a person's risk of having a stroke.
Unfortunately, video and internet games are a distraction for many people in society, not just stroke victims. Many people get involved with social media, video games, or other technology and become obsessed to the point that they don't tend to more important matters such as their health, exercise, school studies, work, family, etc. It can be very challenging to get people off of technology and back into connection with the real world. In addition, when you add a neurological injury such as a stroke, this can affect a person's emotions and behavior which can complicate things even further.
One solution to consider would be enlisting the help of a neuropsychiatrist or neuropsychologist who specializes in working with emotional and mental disorders of those who have had stroke/TBI/etc. Another possible solution is to find games that could help contribute to his rehab. There are video game systems that require larger movement and even video games designed specifically for rehabilitation, so maybe he would be interested in playing some games that would help him physically (and cognitively if needed).
Another possible solution might be getting him enrolled in a neuro day program, where he can go several hours a day and participate in therapy on an outpatient basis. Lastly, maybe he could be motivated by participating in things he likes to do (particularly activities that would get him physically moving, around others and out of the house). You don't mention how old he is, but they may have services he could utilize in his area (adaptive fitness centers, day programs, adaptive sports, etc.)
Partner had a stroke on the right side on brain stem
by Joe
(Tulsa OK)
Question It has been about 2 months since my partner had a stroke. When he had it, the main effects he suffered from it were pretty intense. He couldn’t swallow for a day. He had the hiccups for about 2 weeks straight-non stop. They would get so bad he couldn’t breathe and would be vomiting and trying to catch his breath on top of crying. It was awful. He also couldn’t poop for a week. He kept complaining about an “eye headache “and was really dizzy all the time. And really said he just felt like crap 24/7.
Now it’s like every other day is different. He gets orgasmic “shocks” in random parts of his body that make him all giddy and all of a sudden it turns into the worst “shocking” sensations that make him scream and cry. He wakes up with horrible headaches all the time and is still dizzy almost constantly. But no matter if it’s a good day or a bad day, every night when he goes to sleep he gets sick. Like it hits him in the face with a bat. From the time he lays downs, it’s nothing but moans and groans and he’s freezing. And then he gets nauseous.
Now his swallowing has gone from good to horrible. He sucks it into his lungs or sinuses. We’re both tired and frustrated. Nobody will really explain to us what is happening. And he just tells me he wants to die. I can’t handle this anymore. We’re both getting so depressed and fighting about everything. And nothing is making sense to us anymore.
Answer I don't know if anyone has explained things to you, but strokes can affect people differently depending on where the stroke is located. You mention in your title that your partner had a brain stem stroke. The brain stem controls all basic activities of the central nervous system: consciousness, blood pressure and breathing. All motor control for the body flows through it. It can lead to nausea, vertigo, double vision, and more. The good news is that it has only been 2 months since his stroke, so hopefully he will continue to heal and his symptoms will begin to improve over the next month or two.
I would suggest finding a good neurologist who has experience with brain stem strokes. Many MDs have special interests and not all neurologists will be as experienced with this type of stroke as others. You'll need to be an advocate for your partner right now and insist on help/answers.
Treatment Tips from Others
To see tips from other survivors and caregivers about their treatment recommendations, click here.
Get Our Stroke Rehab Guide

Our stroke rehab guide is designed specifically for patients and caregivers. It's in pdf format and can be immediately downloaded. It includes about
- Stroke Definition & Causes
- Stroke Treatment
- Rehabilitation Information for Physical, Occupational and Speech Therapy
- Exercise pictures
- Q&A from patients and caregivers
- Adaptive Equipment & Techniques
- How to Prevent Another Stroke & More!
Medical Disclaimer: All information on this website is for informational purposes only. This website does not provide medical advice or treatment. Always seek the advice of your physician or other healthcare provider before undertaking a new healthcare or exercise regimen. Never disregard professional medical advice or delay seeking medical treatment because of something you have read on this website. See the disclaimer page for full information.
- Home
- Stroke Questions
- Partner had a stroke on the right side on brain stem