Shoulder Subluxation

Shoulder subluxation is a common occurrence after stroke and can be due to muscle weakness or spasticity. It is characterized by the upper arm bone (humerus) partially dislocating or dropping down from the shoulder socket. The muscles may be too weak to hold the arm bone securely into the shoulder socket or spasticity can cause subluxation by pulling the bone into an abnormal position. Both muscle weakness and spasticity can cause the shoulder blade (scapula) to be abnormally positioned as well.
Initially after stroke, one may experience a flaccid stage where the arm is limp, hangs down, and has no movement. Soft tissue can become overstretched from the effects of gravity and improper handling of the arm. Stroke patients who have their arm unsupported and/or handled inappropriately by caregivers (i.e. pulling on the arm) are at higher risk for traction neuropathy and injury. It is important that caregivers of stroke patients are properly trained in handling the hemiplegic arm especially when shoulder subluxation is present. Lap trays or pillows can provide support when the person is seated and arm slings can be used when the person is standing or walking.
Arm slings are often used on the flaccid arm. Their use, however can have disadvantages such as causing poor alignment and emphasizing positions that can lead to stiffness and contracture so proper fit and directions on use of sling must be accurate. The main uses of a sling for the hemiplegic arm are for support, protection against injury, and to prevent or reduce pain. A sling can be beneficial when out in public because it will alert others not to pull or grab the stroke patient by the arm. Slings are best used during walking especially if for long distances.
It is best to avoid avoid wearing slings that bring the arm across the body with the hand and forearm on the abdomen for prolonged periods. This position is already a problematic pattern for the stroke patient who has muscle tightness and spasticity that bends the arm and pulls it across the body. Wearing this type of sling can contribute to muscle contractures especially if worn frequently. Stroke victims should focus on trying to use their affected arm as much as possible, support their arm when seated, and slings can be worn during transfers or walking. As tone returns to the shoulder muscles, the risk of shoulder subluxation decreases and slings can be withdrawn.
Should I Wear a Shoulder Sling?
Determining if a stroke patient would benefit from a sling is based on several factors. A patient may benefit from the sling if the following are true:
- The sling reduces arm/hand edema.
- The sling improves balance and/or posture when walking.
- The patient does not attend to the affected arm and does not try to protect it.
- The caregiver and/or patient can put the sling on properly.
- The sling helps alleviate pain.
A sling may not be indicated in the following cases:
- The patient has active movement of the arm and the sling hinders this movement.
- The patient is at risk for contractures of the arm due to sling positioning.
- The sling is uncomfortable or causes undue pressure on the neck.
- The sling contributes to unilateral neglect of the arm.
Types of Slings
There are various types of slings for shoulder subluxation. Below are some examples that can be found on Amazon.
The sling below is the type that brings the arm across the body and should be avoided for wearing long periods of time due to positioning the arm in internal rotation across the body. This sling could be used while the patient is up walking for brief periods of time but a sling with better arm alignment (one that does not keep the arm in internal rotation) is preferable.
|
A sling used by some therapists that may provide better positioning of the arm when walking is the GivMohr sling. It was designed by an occupational and physical therapist desiring to develop a more effective positioning device for the flaccid arm. It is meant for stroke patients who can walk or have potential to walk. It's design is intended to reduce subluxation when worn, help with shoulder pain, allow for arm swing, and provide joint compression to facilitate return of movement to the hemiplegic arm. |
|
Other Treatment Strategies
 Shoulder Taping |
Shoulder taping or strapping has been used by therapists, however, research studies are lacking regarding whether taping helps with pain, range of motion, or subluxation of the hemiplegic arm. As a therapist, I have seen some patients acquire pain relief with taping so it may be beneficial depending on the individual. It is best to work with a therapist to determine what type of treatment works for you. |
|
Another treatment strategy for subluxation is neuromuscular electrical stimulation (NMES). NMES involves placing electrodes on the weakened muscles and then using the device to send electrical impulses to nerves. This input causes muscles to contract. This has shown some success with prevention and treatment of subluxation in research studies. Ask your therapist if this type of treatment is appropriate as it may be contraindicated for certain patients (such as those with pacemakers or skin issues). |
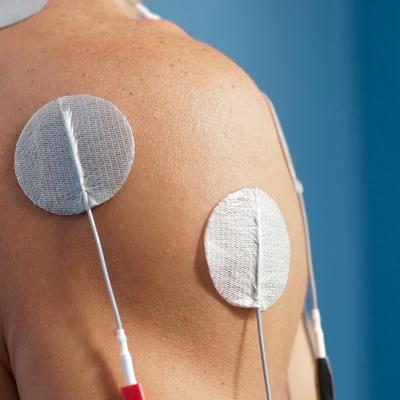 Neuromuscular Electrical Stimulation (NMES) |
Range of Motion

Range of motion of the subluxed shoulder should be taught to the patient and family by a therapist or medical staff. When subluxation is present, it is best to avoid pulleys and uncontrolled range of motion exercises. If the patient has cognitive deficits, neglect, or is impulsive, it would be best to have a trained caregiver to move the hemiplegic or paralyzed arm. Range of motion can help prevent contractures and pain if done correctly.
Arm Trays
Another solutions for subluxed shoulders is to keep the arm supported on a surface such as a lap tray or arm rest while sitting but not across the body and not jamming the shoulder up into the socket. Positioning should be comfortable, emphasize good posturing and provide support. One-arm lap trays can be used on wheelchairs to provide a supportive surface for the arm.
Receive Stroke Recovery Tips, our online quarterly newsletter. Sign up below for free tips on exercises, resources, latest technology, apps, research and more!
To view past issues of Stroke Recovery Tips, visit https://www.stroke-rehab.com/Stroke-Recovery-Tips-BackIssues.html
Get Our Stroke Rehab Guide

Our stroke rehab guide is designed specifically for patients and caregivers. It's in pdf format and can be immediately downloaded. It includes about
- Stroke Definition & Causes
- Stroke Treatment
- Rehabilitation Information for Physical, Occupational and Speech Therapy
- Exercise pictures
- Q&A from patients and caregivers
- Adaptive Equipment & Techniques
- How to Prevent Another Stroke & More!
Medical Disclaimer: All information on this website is for informational purposes only. This website does not provide medical advice or treatment. Always seek the advice of your physician or other healthcare provider before undertaking a new healthcare or exercise regimen. Never disregard professional medical advice or delay seeking medical treatment because of something you have read on this website. See the disclaimer page for full information.
- Home
- Shoulder Subluxation