Submissions from Readers
Stroke Recovery and Lack of Progress After One Month
Question: It has been a month since my mother in law suffered a stroke ... we have a day night nurse plus a helper for her and one of the best physio doctors coming home for a visit everyday ... it has been a month ... no improvement ... her right hand is grade 1 and right leg is grade 3 ... what can we expect?
Answer: Unfortunately, no one can tell you exactly what to expect. A month is very early in the stroke recovery process so you definitely cannot base a prognosis on one month of treatment. Also, it is not unusual for the upper extremity to recover more slowly than the lower extremity in my experience. Your mother-in-law continues to need treatment, and in fact will benefit from having a long term home exercise plan in place even after discontinuing therapy delivered by a healthcare professional.
Stroke recovery for many is a lifelong process. Some will be in and out of therapy over the course of their lifetime. Some information that might help you is to find out from her physician how much brain damage was suffered, what areas of the brain were affected, and if he has an opinion on her prognosis based on imaging studies. Even if you are given a poor prognosis, don't be disheartened. I have seen people achieve way more than they were ever expected to do. I have also seen people who were expected to do well not live up to their potential. It sometimes comes down to a person's will, ability to participate, personality, and the quality of care they receive, not just the amount of brain damage.
One other bit of advice is to make sure your mother-in-law is participating in activities outside of her scheduled therapy visits. One therapy session is not going to make big changes. What will make big changes is to have her constantly working and participating in activities that require her to think, move, and attempt to use her weak extremity. Make sure she is involved in her self care and activities of daily living (ADLs) as much as possible (e.g. helping to dress herself, groom, wash, feeding, etc.) This will empower her which is important. If caregivers do too much for a stroke patient, sometimes the patient will settle into the role of being injured or ill and letting others do too much for them. Even if she can only do small tasks, let her because this is important in her achieving some level of independence.
Click here to read or post comments
Hopeless Hemiparesis
by Jody Jobson
(Bellbird, NSW Australia)
Question: Every health professional I have begged for help with my useless left arm and hand have said there is nothing that can be done and I should accept living without its use. I believe that most in the medical profession accept neuroplasticity is real and achievable, however, I cannot find anybody to help my brain tap into this last ray of hope.
Answer: Neuroplasticity has been studied, and there are certain parts of the brain that have demonstrated this phenomenon, but it has not been identified in all areas of the brain. Therapists often see persons with severe hemiplegia that do not get good return so they work for the best result but also try to prepare the patient for the worst by teaching adaptive techniques. This doesn't mean someone can't get return or that your therapist wants to discourage you. I do think it's important to find a therapist who is well trained and passionate about working with stroke patients, however, to get the best results.
You can look up information on neuroplasticity and see if the particular region where you received brain damage has been shown to yield neurogenesis (new neurons being created). If yes, then that may be promising news to you. If no, then you can still look for research regarding the area of your brain that was affected and see what outcomes for other stroke patients have been.
I often tell patients that tharapy is just an adjunct to recovery. The amount of time spent in therapy is not enough for many people to make significant or lasting gains so it is imperative to learn exercises and activities that you can do daily at home. This is truly the only way the neuroplastic principles will work because neuroplasticity requires much repetition and practice. I suggest you find an exercise regimen that works for you and keep working at it. If you don't have something you do on a regular basis, then contact a therapist that is willing to set you up with a good program. You then can continue to work toward neuroplastic changes on your own (or recruit a friend or family member to help if needed with the exercises).
You can also talk to a neurologist about the extent and location of your brain damage and ask what their opinion is regarding the possibility of neuroplastic changes. Even if they give you a poor prognosis, I think it's still good to continue to exercise the hemiparetic arm even if only passively. The reason I say this is that you never know when a treatment or cure will be found that increases movement so you want to keep the hemiparetic arm in the best condition possible.
Click here to read or post comments
Hopeless Situation?
Question: My 66 year old male friend had a catastrophic left sided stroke last week. Apparently he'd been having "silent" strokes for many years with no symptoms. At present he is has right sided hemiparesis and complete aphasia. The hospital rehab staff told his wife that he would never have any more improvement, would need round the clock care for the rest of his life,and that more rehab would not help. He will never speak or walk again or be able to communicate beyond recognition of 5-20 symbols. Is there no hope for him? She was advised not to seek any other treatment, that it would be futile, and to get used to their new life where she is his caretaker and he will not be able to do anything -eat, use the bathroom, communicate - again.
Answer: Personally, I would never tell someone not to seek therapy and just except the situation. I have seen various families mistakenly told that their loved one would never "walk" or "talk" again. Of course, the severely affected stroke patient may not be anything like they were before, but I have seen patients who were believed to be a "lost cause" learn to walk and speak simple words. As a result, their lives were of much higher quality than if the families had just hired a caregiver and had someone do everything for the patient.
I always take the approach of expect the worst but hope (and try) for the best. I never try to build false hope, but it will not hurt to try intensive therapy for a few months and see if there are any results. If your friend participates in stroke therapy, and he has no improvement, then at least his wife will have the comfort of knowing that therapy was attempted and that she did everything she could to help. I'm sure she doesn't want to live with not trying therapy and then thinking "what if..."
Make sure she finds a very skilled therapy team that is qualified with working with stroke patients. I've seen various rehabs run poorly where the patients are herded through like cattle with very little individualized treatment. All rehab facilities and therapists are not the same. Click on the left hand button on this page about rehab facilities to get more information about finding rehab facilities and therapists.
Click here to read or post comments
why spasticity in my hand (right) does not leave me 3 years after stroke?
by Roman
(CA, USA)
Question: My right hand is still paralyzed after 3 years of my stroke, the arm doesn't move well and the hand doesn't move at all. What can I can do?
Answer: Unfortunately, one can be left with permanent damage after a stroke that can result in paralysis that sometimes doesn't subside. There are various treatments for spasticity (see www.stroke-rehab.com/spasticity.html), however, none of them are full proof. You can try weight bearing, e-stim (if approved by MD and you don't have contraindications such as a pacemaker), robotic therapy and muscle facilitation techniques (e.g. tapping to muscle belly) to try and initiate movement. You can learn more about trying to get hand return by clicking here.
My Weakness is Getting Worst
by Sun Beach
(Birmingham UK)
Question: I suffered a stroke 3 yrs ago. My walking was coming back but the last 2 weeks I've had several persons ask what's wrong with my leg. My left hand is not getting better at all. Please may I have some advice? Thank you.
Answer: I often recommend that patients get follow up therapy after having a stroke. One may initially make progress but then later experience a decline. This is especially true if the person is not following through with an exercise program at home or have had other illness or periods of inactivity.
If you have access to it, I would try to do some type of therapy or even personal training with a qualified person to build strength and endurance. I would recommend doing this every couple of years especially if you are not keeping up with an exercise program on your own or want to change your exercise program to challenge yourself more.
As far as the hand, it can be very tough to rehab especially if one has little or no return of movement. I have answered a few questions that may be helpful to you at www.stroke-rehab.com/stroke-hand-rehab.html that might be helpful to you.
Progressive Weakness After Mom's Stroke
by Julie
(Live Oak, Florida)
Question: My mom had several strokes over the past few years. When she first came home from rehabilitation she was getting stronger. Then out of nowhere, she started growing weaker and weaker. As far as we know, she did not have any additional strokes after they plugged a hole in her heart. She has constant lightheadedness if she holds her head in an upright position. I didn't think stroke victims got progressively worse. No doctor seems to be able to find out why she grows weaker. She is only 69. Any suggestions would be appreciated...
Thank you,
Julie
Answer: Stroke victims can experience multiple TIAs (transient ischemic attacks) or mini-strokes that can cause them to progressively worsen. Dizziness can be a sign of these mini-strokes, and they often are not identified by imaging studies. A physician, however, should probably be able to identify if your mother is having TIAs based on the description of symptoms and other tests.
If TIAs are ruled out completely, then I would look into the cause of her dizziness when holding her head upright. You could read about benign paroxysmal positional vertigo (BPPV) and see if the symptoms of BPPV correlate to what your mom is experiencing. If so, there are therapists who can treat BPPV. Here is a website with information about BPPV: www.dizziness-and-balance.com/disorders/bppv/bppv.html
Something else to consider is where the brain damage occurred. If it occured in an area of the brain that deals with the vestibular system, then chronic dizziness can be a problem which in turn can cause chronic balance issues.
Deterioration
by Steve
(California)
Question: My 89 year old mother had a stroke three weeks ago. While in the hospital she recognized and greeted her children and their spouses by name, and although slurred and not always on point talked in a normal volume and at some length. She is now in a re-hab facility (10 days), no longer greets anyone by name, speaks less (although that has improved a bit over the last few days) and seems more disconnected than when in the hospital. The stroke was fairly severe, right side of brain, full left side paralysis, and the original stroke followed by a brain bleed about 12 hours after entering the hospital. My question is whether it is common for stroke victims to deteriorate and lose certain abilities/behaviors a week to 10 days after the stroke, and if that can reasonably be reversed?
Answer: I have seen some stroke patients worsen, but there is almost always an identifiable cause whether it be another stroke, an extension of the first stroke, seizures, or a medical condition such as dehydration or a urinary tract infection (UTI). I've seen UTIs cause many elderly patients to become very confused and dehydration in a stroke patient can make one appear lethargic and sleepy.
If you have observed definite physical or cognitive changes, and it has been a week or several weeks since her stroke then I would definitely talk to the physicians in charge of her care and express your concerns. Sometimes the physicians are unaware of the changes because they are not involved in the daily care. Sometimes even the nursing or therapy staff may not identify the changes especially if she is in a facility where the caregivers are not consistent from day to day (e.g. different nurses and therapists are working with her day to day). You have to be the advocate for your mom, and don't be afraid to speak up when something doesn't seem right. Also, don't let healthcare workers get away with minimizing your concerns. You know your mother best so you would be the one most likely to know if she is experiencing changes.
Some other issues you might want to look out for are depression and whether she is receiving quality care. You want to make sure that she is getting adequate therapy and not being left in bed too much. If depression is an issue, then talk to her physician about the options of a neuropsych consult or meds.
Click here to read or post comments
Why Did I have a stroke?
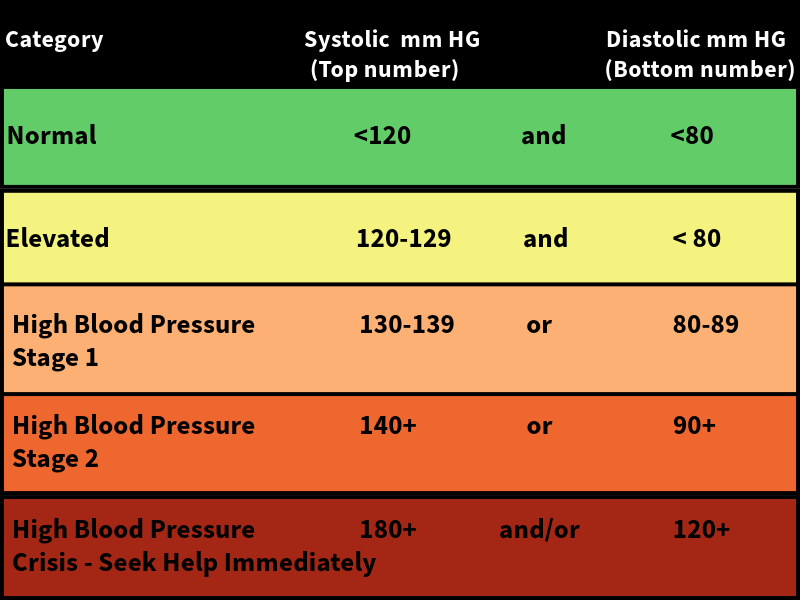
Question: I had a stroke last week, however, I do not have high blood pressure, don't smoke or drink, don't have diabetes, am not overweight, etc. The only thing is strokes run in my family. I just want to know what could of caused me to have two at the same time?
Answer: There definitely can be a genetic disposition to have strokes. If someone has the risk factors you mention above, it just means a person is at higher risk to have stroke. Some persons have high cholesterol due to genetics and most of us form plaque in our arteries as we age which can cause ischemic strokes. Hemorrhagic strokes have been known to affect multiple persons of various ages. Unfortunately, many people have strokes and aren't sure of the cause. I know it feels especially cruel since you have taken care of your body for something like this to happen, however, please continue in your efforts to maintain good health. Once you have a stroke, you are at a higher risk for having another one so it is imperative to continue your quest for good health. God bless you, and I hope you have a full recovery.
77 year old father had massive left hemisphere stroke
by Gabrielle Sommers
(New Jersey)
Question: My father had a massive stroke that had him in a semi-coma. He came out of it and went into a "country club" of a nursing home. He couldn't swallow, is paralyzed on the right side, talking, very difficult, and thinking, reasoning, memory, etc. is very bad. This was August 7, 2012. He now eats 3 meals a day of puree food. He should get his peg tube out soon. Says words, starting to say 2 or 3 word sentences. I have asked him to move his right foot, he did that only a couple of times. He also helps the aide at the home dress himself, pull up his pants, put his shirt on.
He is progressing, and my goal is to bring him home so I, with home health services, can take care of him. The question is, he doesn't really follow directions, he is stubborn also...as old people are, and the nursing home DOES NOT give him physical therapy. They only give him restorative therapy, telling me that he doesn't follow directions so they can't do anything with him. They move his arms and legs in his Geri chair. Sometimes the morning therapy is just him being hoisted from the bed to the Geri chair. They won't use the Electrical Stimulation, nothing. He's in that country club room 24 hours a day as they suck up the medicare. Is that how one treats a stroke like that? I need help! Thank you!
Answer: There have been changes I know with Medicare so I am not up to date on all of the changes. When I worked in a skilled nursing facility, patients were allowed up to 100 days of therapy after a hospitalization, but they had to show progress. If a patient is not showing progress, then the therapists may discharge the patient. I would check with the facility and ask if your father used his 100 days, and if he is eligible to be put back on therapy.
If you think he may qualify, they also have inpatient rehab hospitals that perform 3 hours of therapy a day. If he can't follow directions, it may be hard to find someone to see him for therapy, but I personally think August 2012 is not that long ago and that patients with strokes can change dramatically especially within the first 6 months. I would have an outside person come in and evaluate your father to see if he would qualify for therapy at an inpatient rehab facility. Make sure they know that you are not satisfied with the therapy received at the current facility. You could contact several facilities, and try to find one that would be willing to take him.
It may not be feasible to take him home, but inpatient therapists could help train you in working with him. This would give you a better idea of whether you could take care of him at home or not. Home health is usually only 2-3x/week so I feel he would do better in an inpatient rehab first.
Click here to read or post comments
Sadness After Stroke
by Cindy
(Niagara Falls, New York, USA)
I Get Sad
Question:I get so sad at times like I lost the old me, I was very active and now I’m not, I’ve had a complete meltdown and just sobbed.
Answer: Having a stroke that changes your entire lifestyle comes with a time of mourning. You literally have lost something from your life - the ability to do things as you could before. It is normal to feel sad and to feel loss, but you cannot let this take over your life. These feelings are intense at first and will come and go throughout your life, but if you are unable to return to your prior level of function, you have to figure out how to adapt to the new and become active again in a different way. Some things you can do to help include:
1) Support groups (these can be online, but you may find in-person groups to be better as you can make new friends and interactions) - even if you are only using online stroke forums, it will still help to vent and discuss problems with others.
2) Create a support network of friends and family - if you are unable to drive or take care of yourself, then it's important to have others that can help you. If you do not have someone to drive you, there are often transport services that can. Churches can also be helpful in some instances. In addition, you will want to have friends and family around for social interaction.
3) Take advantage of community resources - transportation, support groups, rec centers, classes for those who have experienced stroke or disability. There are usually many of these programs available and underutilized. If you cannot find resources in your area, contact a social worker at a local hospital for suggestions.
4) If you think you may be clinically depressed and cannot motivate yourself to do anything, then seek out the help of a physician who can help treat the depression (remember, feeling sad is normal, but if it is overwhelming and you cannot function then it's important to seek help).
5) Start a new hobby. Try something new that you have never done before. Maybe it's singing, motivational speaking, helping others, painting, etc. If you can divert your mind to other things or feel like you are contributing to others, it will help you feel better. You have life experiences that can be valuable in helping others!
6) See what others have done - if you can't find motivation in my advice, look for actual stroke survivor stories and see what they have achieved. You will be amazed. There are people who cannot walk, cannot talk, are in horrible pain, etc. that have achieved monumental goals and are so inspiring.
Hopefully, you can get comfort by trying some of these suggestions, but remember that it's okay to be sad sometimes, and these feelings can vary in intensity. However, you cannot afford to let the sadness take over your entire life. I don't know if you are a spiritual person, but seeking God's help can also be life-changing. I am saying a prayer for you now!
Here's a resource you may find helpful for dealing with grief and rebuilding your life after stroke:
https://strokeonward.org/guide/#
Treatment Tips from Others
To see tips from other survivors and caregivers about their treatment recommendations, click here.
Get Our Stroke Rehab Guide

Our stroke rehab guide is designed specifically for patients and caregivers. It's in pdf format and can be immediately downloaded. It includes about
- Stroke Definition & Causes
- Stroke Treatment
- Rehabilitation Information for Physical, Occupational and Speech Therapy
- Exercise pictures
- Q&A from patients and caregivers
- Adaptive Equipment & Techniques
- How to Prevent Another Stroke & More!
Medical Disclaimer: All information on this website is for informational purposes only. This website does not provide medical advice or treatment. Always seek the advice of your physician or other healthcare provider before undertaking a new healthcare or exercise regimen. Never disregard professional medical advice or delay seeking medical treatment because of something you have read on this website. See the disclaimer page for full information.
- Home
- Stroke Questions
- Sadness After Stroke