Submissions from Readers
Spasticity in legs
by Kevin A
(Lake Geneva WI)
Question:Over the last four years I've had several strokes. Due to this I have spasticity in my legs that prevents me from walking any distance at all. I can walk maybe two minutes before my legs freeze up. After that I have to drag my right foot and I am unable to lift my knees. Also it seems that my tendons tighten up behind my ankles to a point where they seem as if they are going to snap.
My neurologist is completely ignoring this. He continues to tell me to continue to walk even when I tell him that I am unable to walk and I describe what is happening. He tells me that it appears that I can walk because I manage to "walk" into his office. He has me walk across the exam room, which is about five feet and he tells me that it looks okay. I can't shop or go for walks or do anything else but he tells me that it looks alright.
For the last four years I was misdiagnosed with diabetic neuropathy and it wasn't until I insisted on seeing a neurologist and got MRI's that I found out all these problems were due to strokes. What can I do? Any information you can offer would be appreciated.
Answer: I would definitely get a second opinion from another neurologist if your current MD is not addressing your concerns. I really urge all patients to be their own advocate. You cannot always rely on medical professionals to listen and address your needs, and it is absolutely okay to seek second opinions. In fact, I encourage it especially in situations where the patient is seeking answers but not getting them.
I have no secret method to get rid of the spasticity in your legs, but I can relay to you information about the different ways spasticity is treated. Everyone is different so what may work for one person may not work from another. Also, some treatments cannot be used on certain individuals due to contraindications. Treatments that are currently used include:
1) Physical therapy including such techniques as range of motion, stretching, strengthening, temporary braces or casts, tone inhibition techniques, electrical stimulation, and biofeedback.
2) Oral medications such as baclofen, imidazolines, benzodiazepines, dantrolene sodium and gabapentin.
3) Botulinum toxin or Botox injections to temporarily paralyze spastic muscles.
4)ITB Therapy - placement of intrathecal baclofen pumps. Intrathecal Baclofen is delivered directly to the spinal fluid and usually has less side effects that oral baclofen.
5) Surgery such as selective dorsal rhizotomy which involves cutting selective sensory nerve roots.
My advice is to talk to another neurologist and discuss the treatment options above to decide if any would be appropriate for you.
Click here to read or post comments
Spasticity Problems After Stroke
Question: What exercises may help if a patient cannot raise the palms of his hands e.g. to say goodbye of as if to give a blessing? The patient cannot unfold his hands on his own either.
Answer: I recommend stretching the fingers out and then placing them on a surface to do weight bearing through the hand. If the fingers can be stretched out enough for the hand to be flat then you can place the hand on a book, table, or mat, and have the patient lean over the hand putting weight into the arm (a caregiver can block the elbow if it tends to collapse). This helps decrease the spasticity.
If the hand cannot be stretched out enough to be flat then place it on a curved surface instead such as a soccer ball. Then have the patient bear weight on the ball or the caregiver can raise the ball bending the patient's wrist back and have the patient try to push the ball away while the caregiver is holding it. This provides stretch and weight bearing to the hand and wrist.
Once the hand is stretched and spasticity is decreased, have the patient try to lift the wrist back on his own several times. If the tone increases again, go back to weight bearing to decrease the tone and have the patient try to lift the wrist again. Also have the patient try to open the fingers. If the patient is unable to lift the wrist or open the fingers, tap the back of the forearm to help elicit the movement.
If the patient has no contraindications, electrical stimulation can be used by a therapist to help stimulate the muscles that open the hand. Talk to the patient's therapist to see if getting a home e-stim unit would be an option.
There is also a rehabilitation device called the Hand Mentor that can be found in some clinics. The Hand Mentor encourages self initiated movement in the wrist and fingers and assists movement only when necessary. The Hand Mentor has three different program types which are designed to reduce spasticity, improve motor control and recruit specific muscle groups. This device would only be offered in a therapy clinic, however.
Click here to read or post comments
SPASTICITY ON LEFT LE
by Mary
(Chicago, IL)
Question: I have a patient with a grade 3 spasticity on B UE/LE and the patient cant hardly stand up and maintain balance due to left hip and knee flexor synergy. What type to brace I can recommend on him?
thanks,
Mary
Answer: Unfortunately, my expertise is not in leg braces. I know in reading literature that bracing can be difficult when trying to improve gait with flexion synergy in the LE. I am not able to recommend a brace to improve gait and standing, but I would consider knee bracing/splinting to prevent contractures if knee flexion is a problem at other times besides when attempting to stand. There have been some positive studies when using e-stim in addition to splinting if done on a regular basis. I generally use progressive dynamic splints on the upper extremity.
One activity you might try is applying an air splint on the flexed knee when attempting to stand. This might allow for some increased weight bearing and tone reduction on that side and would also free up your hands to help with hip and trunk posture. The patient could then attempt shifting weight side to side, lifting the stronger leg (i.e. on and off a step), or side stepping allowing weight bearing on the weaker leg. The air splint is not meant for gait as it will interfere with the gait pattern but definitely could be using for standing exercises. Obviously, I do not know your patient, but I suspect if the knee and hip are flexed, there is very little weight bearing going on in standing. Weight bearing can help reduce the spasticity as you probably know.
If you have any reputable bracing/splinting representatives that you deal with (I recommend that they have a clinical background), I would ask for their opinion.
You can do a search online for air splints if you're interested in purchasing one. Below is an example of an air splint on the arm.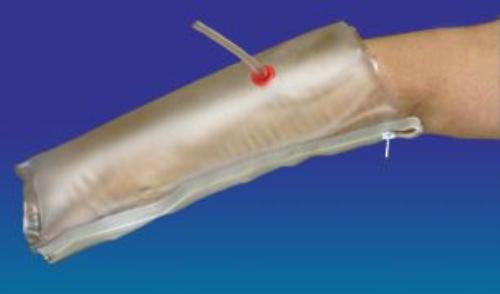
Decreasing Tone
by heather
(wellsville,ny)
Question: Does mobilization of the trunk result in a decrease of tone in the arm and should it be done prior to weight bearing with the involved arm?
Answer I always perform mobilization of the trunk prior to weight bearing with the involved arm. Muscles in the trunk and surrounding the shoulder blade (scapula) often have tone or are shortened/elongated due to muscular imbalance caused by the stroke.
If you mobilize the trunk first, mobilization of the shoulder blade will be easier which in return allows for improved range of motion in the shoulder and arm. This is the sequence I follow when trying to reduce tone in the arm:
In a lying position on the back:
1) Trunk & pelvic mobilization (one way to do this is have the patient bend their knees with feet flat on the bed and take the knees side to side and then practice rolling toward the involved side). Make sure you have a therapist show you how to do this safely before trying it on your own.
2) Scapular mobilization (shoulder blade)
3) Stretching of the shoulder, elbow, wrist & hand
I then have the patient come to a sitting position and do the following:
4) Trunk and scapular mobilization in sitting
5) Weight bearing of the hand and arm
I plan on adding examples of these exercises as well as others as I expand this website. You are welcome to subscribe to my RSS feed which will let you know anytime I update or add to my site.
Spasticity, Botox, and Phenol Injections
by Gilbert
(Prospect Park, NJ )
Question: Is botox or phenol therapy a good idea for a stroke survivor?
Answer: Botox and phenol can be injected into specific muscles to reduce spasticity. This reduction in spasticity can be beneficial allowing increased range of motion for activities of daily living or potentially allowing for more active movement. These treatments can be highly effective for some and less effective in others. A physician experienced with botox and phenol injections can determine if a stroke patient is a good candidate for these treatments.
Adverse reactions to botox can include nausea, fatigue, bronchitis, muscle weakness and limb pain. Botox has been approved by the FDA for treatment of spasticity in the elbow, wrist, and fingers in stroke patients (specifically the flexor muscles). Botox comes with a warning that it is produced from the same bacterium that causes botulism and has the potential to spread beyond the treated area and cause symptoms similar to botulism. Side effects from phenol can include pain and burning/tingling and swelling of the injected area.
Botox and/or phenol may be beneficial for individuals having problems with spasticity and these options should be discussed with a physician.
Click here to read or post comments
Ankle Spasticity After Stroke Due to Venous Sinus Thrombosis
by Rahul
(Mumbai)
Question:My mother suffered from stroke following venous sinus thrombosis. She has recovered well and now the only problem area is her ankle, which is still spastic. Dorsiflexion at ankle is difficult and it goes into external rotation can you suggest some exercises to tackle that?
Answer: Ankle spasticity can be approached in several ways. Here is a list of treatments ranging from conservative in nature to surgical techniques:
1. Daily stretching - stretch the ankle into dorsiflexion until the point of discomfort and hold for 60 seconds. Repeat twice daily.
2. Range of motion exercises - foot circles rotating the ankles one way then the other, raising the foot off the floor (ankle dorsiflexion), rock back and forth on the toes then heels in a standing position (support hands on wall), and trying to pick up objects such as marbles with the toes. Perform 10 repetitions of each exercise twice daily. Equipment can be used to help with stretching and exercises such as a foot rocker.
3. Electrical stimulation (e-stim) - this technique can be used on some patients as long as they don't have contraindications for use (check with MD to see if patient is a candidate for e-stim). E-stim may help reduce spasticity as well as strengthen weak or spastic muscles.
4. Splinting - an ankle foot orthoses (AFO) can be made to position the ankle and keep it on a static stretch. Dynamic splinting (splints allowing ankle motion) and serial casting are also available.
5. Medication - various medications can be administered by a MD to control spasticity. Examples of such medicines may include baclofen, dantrolen sodium, and Zanaflex.
6. Nerve Blocking Injections - examples include phenol and botulinum toxin.
7. ITB - Intrathecal Baclofen Pumps can be surgically placed to deliver baclofen into the subarachnoid space of the spinal cord to help reduce spasticity.
8. Surgery - One common surgery technique includes an anterior tibial transfer to help straighten and balance the foot. A more extreme surgery is a dorsal rhizotomy which involves disrupting the nerve supply to the muscle.
Tone
Question: My 5 yr old had a stroke 8 mos ago. She has produced quite a bit of tone in her left hand sometimes making it difficult to open her hand, grab and release objects. The OT said that once tone sets in you cannot get rid of it. Is this true? This is the first therapist that has told me this.
Answer: I have seen stroke patients go through stages of initial flaccidity, increasing tone, and then into more normal movement so I don't agree that once tone sets in, you cannot get rid of it. However, I will say that the persons I have seen overcome tone usually do so in the first few months after stroke. This is not a proven fact but just my own personal observation with patients. Patients that I've seen with high tone for an extended period of time often do continue to have problems with tone.
From your post, it sounds like your daughter is able to grasp and release objects at times when the tone is not too high. The good thing for you to know is that there are ways to manage or decrease tone allowing for more functional movement in those that do have movement present. A technique that I teach patients to help control the spasticity is weight bearing. Though weight bearing does not get rid of tone, it often will lessen it so that the patient can move more freely. I would ask your therapist to show you ways to manage your daughter's tone and also teach those techniques to your daughter. Hopefully that will enable your daughter to relax the hand enough for improved grasp and release. Sometimes it works and sometimes it doesn't.
There are also medical means to control spasticity that work for some but not for others. My experience is with adult clients so I don't know if all the same options are available for children. You can read about various medical management strategies for spasticity at www.stroke-rehab.com/spasticity.html
Spasticity is really just managed or controlled at best in most cases. Spasticity that subsides in some patients in my opinion appears to occur as part of the healing process. After the acute healing has occurred and tone is still present, it often continues to linger in my opinion. Please note that this is only an opinion from my observations with stroke patients. My advice to you is to ask your daughter's physician about the prognosis for tone and to learn spasticity inhibition techniques from the therapist to help your daughter manage the tone as best she can.
Stiffness in Leg
by Garry
(62037)
Question: I was walking pretty good with a quad cane,but now it seems like my leg is getting stiff at knee and up by my groin Also my foot feels like needles ar sticking in the bottom when I take a step.
Answer: Stiffness could be a result of spasticity in the knee and groin. Range of motion activities and stretching for the leg might be helpful if this is the case. You can have your MD evaluate to see if you have increased spasticity. The level of spasticity often changes during the stroke recovery process so it can take an individual by surprise.
The pins and needles feeling you are experiencing in your feet is most likely paresthesia. Paresthesia is a pins and needles feeling that can be chronic or temporary. It can also come and go after stroke so the outcome is hard to predict.
Sometimes stroke victims experience central pain syndrome post stroke. Central pain syndrome can occur due to damage to the brain and can occur immediately or months after the stroke. Pain may be constant, made worse by touch or pressure, and be sensitive to temperature changes. The pain sensations are often described as pins and needles, burning, or sharp pain. There may also be numbness associated with the pain.
These are just a few of the problems that can occur post stroke. I recommend making an appointment with your neurologist to determine the cause of your onset of stiffness and sensory issues as well as to determine if it can be treated.
Spasticity problems
by Arno Pieterse
(Port Elizabeth , South Africa)

Question: I had a stroke 06 March 2012. After 7 months I start to have spasticity problems . I walk everyday about 400 meters , but stay stiff. Will the stiffness go away and after what period?
Answer: Hi Arno. Unfortunately, only time can tell if the spasticity will go away or remain with you. The longer you have it, the less likely it is to go away on it's own. It is important to stay active and stretch. If the spasticity is interfering with your activity, you might want to talk to your MD about medicine options if you haven't already. You might look into massage therapy as well. It won't get rid of your spasticity but can help with tight, tense muscles which may relieve some of your discomfort.
Treatment of Flaccidity and Spasticity After Stroke
by puja
(MP)
Question: What is the role of ice in treatment of the flaccid condition of stroke? Please describe in detail. Also, what is the treatment for the spastic stage of stroke?
Answer: If the doctor gives the okay, ice can be used to help with swelling in the hemiplegic hand. Usually the procedure involves dipping the hand two to three times in ice/water for 5-10 seconds and repeating a few times throughout the day. You could try this technique for several days and see if swelling decreases. The key points to remember though are that you need physician approval, only leave the hand in for 10 seconds at a time, only perform the technique 3-4x throughout the day, and discontinue if there are any problems or no results are seen. One has to be careful when using ice with the hemiplegic hand because the stroke patient often has decreased sensation so close supervision is needed as well as physician approval.
Ice can also be used to facilitate muscles by briefly rubbing ice for a few seconds over the muscle you wish to facilitate (e.g. triceps to extend the arm and back of forearm to extend the wrist/fingers). I prefer tapping as my method of facilitation rather than ice.
The best treatment for the flaccid arm and leg is weightbearing, passive range of motion, proper positioning of limbs, and facilitation techniques such as tapping, quick stretch, and electrical stimulation (physician approval required for electrical stimulation, and pt. must have no contraindications).
The spastic limb also requires weight bearing which helps with stretching and reducing tone. Scapular mobilization is important during the spastic stage to help reduce tone and increase shoulder range of motion. For more information on treating the flaccid limb, see the links below:
www.stroke-rehab.com/hemiplegia.html
www.stroke-rehab.com/hemiplegic-hand.html
www.stroke-rehab.com/stroke-recovery2.html#how to improve stroke
www.stroke-rehab.com/shoulder-subluxation.html.
For information on treating spasticity, see these links:
www.stroke-rehab.com/spasticity-and-stroke.html
www.stroke-rehab.com/spasticity.html
Spasticity in the UE
Question: I have a patient with abnormal flexor tone in the left affected UE. She has increased flexor tone in the biceps and fingers and presents with her elbow and wrist in the flexed position. It is believed she is in stage 2 of brunnstrom. She also has shoulder subluxation greater than 2 fingers and trace muscle contraction of the upper traps. She is currently receiving inpatient rehab services. Her CVA was in the R basal ganglia. What weight bearing activities and interventions would you recommend for her three week stay?
Answer: This sounds like a question I would have been asked in therapy school. I'm not going to give you a textbook answer but rather what I would do based on my experience. Since the shoulder is subluxed, I would make sure the arm is supported when sitting (tray or lapboard)and standing/walking(can use a sling when standing). I am not a fan of the slings that hold the arm across the body as they emphasize the flexor spasticity pattern, but they are okay to put on the patient for short periods when walking/standing. Do not leave this type of sling on the patient in a chair because the patient will become stiffer and lose range of motion if kept in this position frequently. I would also try kinesiotaping the shoulder for extra support. I would initiate e-stim for subluxation if the patient did not have any contraindications for e-stim and the MD was in agreement. I would also teach the patient and caregiver how to do gentle passive range of motion and educate them on how to protect the arm. I would do range of motion to the arm as well within patient's pain tolerance and using appropriate techniques (making sure the shoulder blade is rotating and approximating the humerus to reduce subluxation).
Since the patient only has a short stay in IP rehab, it is imperative to teach them (and their caregivers) compensatory techniques for ADLs and educate them on equipment that is available. This would include one handed techniques and equipment for dressing/grooming/feeding etc. It's also important that the patient knows how to transfer safely or has a caregiver that has been trained to help with the transfer if the patient is unable to do it herself. One component that is highly missed in IP rehabs is caregiver education. Please educate and also refer the caregiver to websites so the caregiver can prepare for bringing the patient home or start looking at other facilities if home is not an option.
I would also begin to do weight bearing activities with the arm in sitting to decrease tone and see if the patient can hold the arm in place or use it for support. One of the first things I try to teach my stroke patients is being able to place the hand and keep it on an object. I usually start with the patient trying to hold the hand on a mat then progress to see if the patient can keep their hand on a ball (e.g. soccer ball) without it falling off. If the fingers will not lie straight on the mat, you may be able to get the fingers to lie open on the curved ball. Once you get the fingers open on the ball, you can also apply gentle pressure to the hand to push it back into wrist extension and stretch the forearm flexor muscles. I also will place the patient's hand on a cane and see if they can push/pull the cane forward and back. I will assist the hand to stay on the cane if needed.
I also use facilitation techniques (and e-stim if appropriate) to try and elicit movement. Some of the facilitation techniques I might use would be tapping, stroking or vibration to the muscle belly. I have good results with eliciting elbow extension when tapping the triceps (with the patient lying on their back and the shoulder supported at 90 degrees of shoulder flexion which increases extensor tone). If you can elicit any movement, this will often excite and motivate the patient to try harder.
So in review, what I would do in my practice is:
1. Attend to the subluxation and train patient/caregiver to handle the arm
2. Teach patient and caregiver how to transfer and use compensatory techniques for ADLs
3. Use weight bearing activities as described above
4. Try to elicit movement through facilitation techniques.
Walk Aide after Botox to treat spasticity for foot drop in stroke victims
by Melanie
(Tucson, AZ USA)
Question: Are devices such as Walk Aide or Bio Ness 300 necessary after Botox treatment for foot drop/spasticity in elderly stroke victims?
Answer: I wouldn't say that these devices are necessary after botox treatment, but they can definitely be beneficial. Patients considering these devices should receive a trial run during therapy to determine if the device is right for them.
does botox help in an arm and leg?
by PAULINE
(TROY, MO)
Question: Does botox help in a person's arm or leg? I had it in my arm 3 weeks ago with therapy following, and there is no improvement. My stroke affected my left side.
Answer: From the EVIDENCE-BASED REVIEW OF STROKE REHABILITATION Executive Summary (15th Edition:
"There is strong evidence that
treatment with botulinum toxin
significantly decreases spasticity in the
upper extremity in stroke survivors
and that this is associated with
increased range of motion. There is
moderate evidence that electrical
stimulation combined with botulinum
toxin injection is associated with
reductions in muscle tone."
So what that means is that botox injections have been shown to decrease spasticity and improve joint range of motion. However, that does not mean the patient has improved functional use of the arm. I have had patients whose fingers were curled tightly and their elbows bent due to spasticity who responded well to botox injections in the sense that their hands were no longer fisted nor their arm drawn in. However, they did not necessarily gain any functional movement. Botox treats the spasticity, but this does not mean the arm will move on its own volition or be functional. It just means that the spasticity has been decreased so that one can attempt to move the arm and use it.
Longterm post stroke progress potential
by Peter Markie
(Hereford England UK)
Question:Dear Sir/madam,
My name is Peter Markie a former UK Paratrooper who sustained a closed head injury following a boxing match in Belfast in 1990. I curently live in Thailand where I recieve lots of thai yoga massage weekly. I would be very very happy indeed if you could answer me a question which would be like winning the lottery for me if it can be confirmed. I have been disabled post trauma for a long time now and I think I may have been thinking on the wrong lines for all of these years in the respect of my rehab program having learned things recently through online research about neuroplasticity and the brain and body's innate wisdom and capabilities for relearning. My tendencies have been to overly worry about pushing myself too hard physically believing if I do so I will just keep getting tighter and stiffer. My recent learning after all of this time tend to indicate that the weakened muscles must be worked to their limits and eventually the muscles and nerves relearn the movements and can do them in a more relaxed and natural way in time after great effort. I have always been worried about pushing my left side too far because of the tone increase but like I have stated earlier I have been reading articles saying that the stiffness and tone needs to be worked through over time and even with long term post stroke. Could you please offer me some reassurance that if I continue long term with a stringent rehab program that it is still possible to regain some more movement and be a little looser in time but mainly I need to know if I can work my left side to a high percentage of effort and in doing so will not be creating more problems with tonal increase. Thank you so very very much for your help and I really do hope you can offer me some encouragement. Kindest regards,
Peter Markie
Answer: I really couldn't comment on if your specific routine is helpful or safe since I am not your therapist and do not know your condition, but I can tell you that according to results from research, weightlifting does not increase spasticity. You do need to be careful though about not lifting too heavily, tracking blood pressure changes, and using proper breathing as heavy weightlifting does have stroke-associated risks. Here are a couple of articles/references you can read about weightlifting and stroke:
http://www.strokeassociation.org/STROKEORG/LifeAfterStroke/RegainingIndependence/PhysicalChallenges/Weight-Training-After-Stroke_UCM_309780_Article.jsp
http://online.wsj.com/public/resources/documents/hb2.htm
http://strokengine.ca/intervention/index.php?page=topic&subpage=quick&id=50
Click here to read or post comments
shoulder pain after a stroke
by aditi
(los angeles)
Question: My mother suffered a right CVA about a year and half ago with left sided weakness. Her left arm is very spastic and non functional. She has severe shoulder pain , almost chronic. What can we do to to relieve her of this pain?
Answer: I would consult with a physician regarding options to address the spasticity which in turn may help relieve the shoulder pain. You can view more about spasticity treatment options at: https://www.stroke-rehab.com/spasticity.html .
Click here to read or post comments
Problem with Cold
by Mike
(Shreveport la)
Question: Had a mini stroke 3 months ago! Left side affected. All came back pretty good but noticed in cold weather it's difficult to use hand .. and leg feels heavy.
Answer: I don't know if you have any spasticity, but cold weather can increase spasticity which can in turn make it harder to use the the muscles involved. If you don't have any issues with this, it may just be your body's normal reaction to the cold. The body attempts to heat the core when it's cold outside and blood flow to the hands and feet is reduced. This can have the effect of making the extremities feel more clumsy. Maybe this effect is more noticeable to you since having your stroke.
Click here to read or post comments
Spasticity Problems
by Erin Franklin
(Danville, Virginia)
Question: I had 3 mini-strokes 3.5 years ago. I have regained partial use of my left arm. I have been experiencing what my therapist calls "tone". My doctor said mini-strokes do not cause loss of use of the left arm and she is reluctant to continue referring me for physical therapy. I am in a lot of pain. How do I convince her I need help? I did not diagnose the mini strokes myself, neurology told me after they did an MRI. I am using the veteran's hospital and I cannot afford the therapy.
Answer: Mini-stroke is a term that usually applies to what medical professionals call TIAs or transient ischemic attacks. TIAs, however, are temporary (no disability noted after 24 hours) and do not result in permanent damage to the brain or in permanent disability. With that said, it sounds like what you are describing is not a TIA but maybe small strokes (meaning a small portion of the brain was affected). There has been research that has shown also that it's not the size of the stroke that matters but where it occurs. I think you should get a copy of the results of your MRI which will most likely show if you had strokes. If so, I would give this information to your MD and tell him/her that you did not have a TIA but a stroke that left residual damage in the brain as the two are different. Do not use the term mini-stroke as this is thought of as a TIA which is not suppose to cause permanent damage (unless of course you did only have TIAs, but this is doubtful since you have loss of use of your arm and spasticity). You can always visit with another MD as well for a second opinion.
Does Ice Therapy reduce spasticity?
by Rajeev
(Pune, India)
I had a stroke in February 2013. i had undergone carotid enderectomy.
since the stroke, my left hand is spastic & I also had footdrop in my left leg.
One of my physiotherapists suggest stretching the arm whereas another is treating me with electrical simulation for scapula & tricep (he wants to break the synergy in the bicep).
Some other specialist suggests to massage the hand, whereas, both the physiotherapists seems to be dead against the massage therapy. I do not know the reason of their resistance though! At this juncture, I am totally confused.
I would like your kind suggestion about the course I should continue along and also your comment on probable time for complete recovery suggest.
Thanks & Best Regards,
- Rajeev
Answer: According to the evidenced based review of stroke rehabilitation (www.ebrsr.com), there is moderate research evidence from one “fair” quality study that massage therapy reduces pain and anxiety levels post-stroke. There was no mention of the effect of massage on spasticity, but I see no reason why you could not try massage and see if you get positive results (as long as your doctor gives you the okay). I've had several patients who have tried massage therapy and like it.
In your title, you mention ice therapy but do not talk about it in your question. Ice has been shown to help reduce spasticity in some research studies, so it may be helpful to apply an ice pack prior to physiotherapy.
Spasticity of left leg
by Connie
(Arlington, Tx)
Question: Does sitting with weight mainly on the right hip cause spasticity problems to the left leg?
Answer: Each individual stroke patient can have movement patterns or positioning that can increase (or decrease) tone. It is recommended to have a patient as balanced as possible when sitting with equal weight over both sides of the pelvis (or hips). Seating or positioning devices are needed in some cases to achieve this. Balanced sitting will help prevent shortening and tightening of certain muscles while preventing overstretch and weakness in other muscles. If you suspect sitting posture is affecting the left leg, you can reposition the patient in better pelvic alignment and see if lower extremity tone normalizes. If the patient is in a wheelchair, I suggest seeing a seating specialist to make sure the best postural alignment is achieved.
spasticity over time
by Jon Turner
(Canton, GA)
Question: I am a 44 year old stroke survivor. I am 4.5 years post stroke. I can walk pretty well, but my gait is a bit 'off' because of spasticity in my left(affected) leg. Gives me a stiffer gait pattern.
Does spasticity generally increase, decrease, or remain constant as time passes? or is there a common pattern at all?
Answer: I haven't read any research that talks about what happens to spasticity over the long term. That doesn't mean it doesn't exist - it just means I personally have not read any. Spasticity can definitely change in the earlier stages of stroke, but in my rehab experience, I haven't seen any patterns of change in spasticity several years post stroke unless it was in response to something like receiving some type of treatment (e.g. botox) or change in medical status. There are things that can affect spasticity in the short term such as positioning, stress, illness, increased effort, and so on, but these changes are temporary effects. Muscles can shorten over time, however, which can cause shortening and contractures. This could be perceived as a worsening of spasticity even though it is actually due to physiological changes in the muscle length.
2 yr old stroke with increased spasticity of hand/fingers
by Deborah Garcia
(Justin, Tx)
Question:What type of splint is appropriate for contractures and weakness? Fingers are flexed and adducted. what are some good compensatory strategies? handwriting with non-dominant had is hardly legible. Trouble with clothing fasteners too.
Thanks for your help!
Answers: Contractures are best treated with a splint that provides a low load prolonged stretch. This means a splint with light pressure or load that is used each day for an extended period of time. Splinting when spasticity or excessive tone is present can be tricky if tone fluctuates because what may be a light stretch when you apply a splint may become too much of a stretch/pull as tone increases. I would consult with a CHT (Certified Hand Specialist) with is either an occupational or physical therapist that has a specialty certification in working with hands. They are experienced in making splints. You could also look into the Saebo stretch splint (http://www.saebo.com/products/saebostretch/). Saebo also has the Saebo Flex which can help assist with opening the hand when practicing grasp/release, but you would need to be evaluated by a therapist trained in using Saebo to see if you were a candidate.
Also, if you want to learn to write with the non-dominant hand, there is a book call Handwriting for Heroes that was designed for members of the armed services that lost their dominant hand during their service. It teaches one how to write with the non-dominant hand in 6 weeks with a carefully laid out plan.
leg muscle tightness without loss of movement
by Susan Wilson
(Arcata, CA, USA)
Question:I experienced a mild CVA two years ago, affecting a 7mm spot in my brain, according to my MRI. Fortunately, it only affected the sensations in my left side, waist down, without residual pain. I have full use of the leg and no spasticity (i.e., no abnormal movements). Brief physical therapy was unproductive, since the 'fault' is in my brain, not my leg muscles.
The chronic sensation I now experience is a tightness, more in some areas than others, as if the leg is wrapped in a tight elastic bandage. Lately, however, it has become even 'tighter,' and taking walks is not enjoyable, limiting my exercise options (I do still take aqua aerobics classes every week).
Again, I know I am fortunate to have such mild aftereffects of a CVA, but was just wondering if anything can be done to improve the situation. Thank you so much, Susan Wilson
Answer: You might want to try graded motor imagery and mirror therapy if you haven't already. These techniques have been successful in relieving problems with phantom limb pain in amputees and have been useful in pain syndromes with stroke patients. I know you described the sensation as tightness and not pain, but I still believe trying these techniques may be worth a shot. The premise behind using these techniques would be to make neuroplastic changes in the sensory cortex of your brain. You can visit the website http://www.gradedmotorimagery.com/ to learn more about these techniques.
Click here to read or post comments
Spasticity in the left hip and lower back pain
by Michelle
(California)
Question: Hi, I am a 51 year old female who suffered 2 left brain strokes and 1 right brain stroke 3 months ago. I have no paralysis, only right side weakness and some numbness. Rehab is going well so far. I have had back pain since the strokes if I walk or do any activity on my feet (e.g. ADLs or simple household chores), I get back pain. Usually if I sit down for 15 minutes, I can then continue activity for 15 more minutes then I have to sit again. Sometimes I can't even sit up because the pain is so bad. Does anyone else have this type of hip and back pain? I do stretches when the pain is bearable. It seems to be getting worse. I have been in bed for 2 days and now can barely get up to the toilet, and when I try to walk my leg feels like it doesn't want to bear weight. So much pain can't even get in the car to go to doctor or PT. I'm currently trying ice. Any suggestions? Feeling desperate.
Answer: Having this type of pain is not normal, and you definitely need to get in to see a physician to find out what is causing the pain. There are some pain syndromes that can occur after stroke, but you could also have something wrong with your back or hip. In order to treat the pain, you have to find out if it is the result of the stroke or some other ailment/injury. Hopefully, you will be able to get to a physician's office, but if you stay unable to get out of bed or get to a car to see a physician, then I would call emergency services to transfer you to a hospital. When getting evaluated, ask if they can rule out back/hip issues with some type of x-ray or scan if possible. Sometimes when you have a stroke, medical professionals will tell people that whatever is wrong with them is due to their stroke without doing a thorough evaluation. Just because you had several strokes a few months ago doesn't mean your current pain is from those strokes. It may be because of the strokes, but it could be due to other causes that have just been exacerbated by the strokes and their effects or it could be something different altogether. If other problems are ruled out, and it is determined the pain is due to the stroke, I would suggest seeing a pain management specialist or talking with a neurologist about treatment options. Non medication options for pain would include modalities like heat/ice packs, stretches, exercise, massage or using a Tens unit if approved by MD.
spasticity problems plus much more
by Anne.
(Australia)
Question: My friend, Kerri-Anne, has what she refers to as "blobs" on the hypothalamus. She had a massive bleed about 10 years ago. It left her with the same symptoms as a stroke, with little balance, poorly functioning right side. For 6 months she lost much of her sight (which then returned but fluctuates). There are times when she has such bad spasticity in her right foot she cannot wear shoes for months. There are days when I speak to her and her words are slurred and she has trouble with pronunciation.
She was never sent to rehabilitation. I enrolled her in water aerobics in 2009 which has been of great benefit. However, she cannot attend on a regular basis.
Is it too last to rehabilitate and address the above issues? If it is not too late, what home based exercises can she do, especially for the spasticity in her foot.
NB Kerri-Anne continues to have slight bleeds, normally just before menstruation and when under stress.
Thank you for your time.
Answer: A lot of spontaneous healing occurs in the first year after stroke and then recovery tends to slow down dramatically, but if she has never had rehabilitation, I definitely think she could benefit. I would actually see if she could get doctor orders for therapy and then have a therapist set her up on a home exercise program. You can read about questions I have answered regarding spasticity at: https://www.stroke-rehab.com/spasticity-and-stroke.html.
As a quick review, some things that can be used to help spasticity are cold, massage, medicine, botox, e-stim and orthotics.
Extensor tone
Question: I was told I have extensor tone, but I'm confused as to what that is. Does it mean that when I extend my fingers there is tone or does it mean that at rest my fingers are extended. I've heard other therapist's talk about flexor tone. What's the difference?
Answer: Excessive tone or hypertonia is when the muscles have too much muscle tone and may become stiff and difficult to move. Extensor tone refers to increased tone in the muscles that perform extension. Some examples of extensor muscles are your triceps that straighten the elbow or the quadriceps that straighten your knee. Flexor tone refers to increased tone in muscles that perform flexion. Examples of some flexor muscles are your biceps which bend your elbow, various forearm and hand muscles that bend your fingers or the hamstrings which bend the knee. One can have excessive tone at rest, and it may increase with movement. With extensor tone at rest, your fingers would tend to want to stay straight and trying to bend the fingers would be more difficult.
Sometimes, you will hear therapists talk about spasticity which is a particular type of hypertonia that is dependent on movement and velocity. With spasticity, muscle tone increases with passive movement (e.g. stretching) of a body part and is velocity dependent (faster passive movement results in higher muscle tone/resistance). With spasticity, patients usually have exaggerated reflex responses. With extensor spasticity, if someone tried to bend your fingers, the fingers would try to extend, and the faster someone tried to close them, the bigger the extensor response would be.
Spasticity
Question: I have spasticity in right arm and when I walk my elbow does nor want to lie straight. My right hand the index finger does not flex however my thumb and third finger function pretty well I have had botox injections but they don't seem to do much. I think the doctor is not injecting in the right places she doesn't seem to care if it works or not and says Botox does not do much.
I have tried to explain where the muscles feel tight but she will not inject there.
I am wondering where the injections should be placed to help me with straightening my elbow and index finger
Thank you
Answer: Botox Injections to help with elbow flexor spasticity should be placed in either the biceps, brachialis or brachioradialis muscle. I would seek a second opinion or find another MD to do the injections if you are not satisfied with your current MD.
spasticity problems
by Val Jones
(Chicago, IL)
Question: How can I correct my spasticity, balance and initiation of walking upon standing? I had a hemorrhagic stroke.
Answer: You can read about spasticity at https://www.stroke-rehab.com/spasticity.html. For some ideas on how to better initiate standing, you can read https://www.stroke-rehab.com/strength-exercises-to-get-up-from-a-sitting-postion.html. For ideas to improve balance, visit https://www.stroke-rehab.com/balance-problems.html.
Spasticity of neck after a stroke
by Jay Katz
(Pittsfield, MA)
Question: Hello, my name is Jay Katz. I had a stroke eleven years ago and I still am unable to walk. My right side is ataxic, but not spastic. There is a a lot of spasticity in my neck however. After my stroke and before I had Botox injections in my neck, my chin (and my head) was always in my chest due to the spasticity of the muscles in my neck. It hurt to lift my head due to the spasticity in my neck. After nine months I got Botox injections in my neck. They definitely helped me. I could lift my head for the first time since my stroke. I have gotten Botox injections every 3 months since. Last year however, I went a span of five months before I got Botox injections in my neck (due to a change in doctors). Ever since then, I still get Botox injections in my neck but they don't seem to be as effective. My head is starting to slide back in my chin, due to the spasticity in my neck. I do neck stretching exercises every day in between Botox injections. My doctor has increased the dosage of Botox when he injects my neck, but nothing seems to work. My head is starting to slide back into my chest. Either I went too long between Botox injections or my body has built up a tolerance to the Botox, or both. Has anybody under gone a treatment that is effective against spasticity other than Botox injections?
Answer: You mentioned that you changed doctors whenever you noticed a change in the effectiveness of the treatment. I'm wondering if it possibly could be as a result of difference in injection technique (or which muscles/sites were injected)? Maybe you could check with your first doctor or the office records to see if there is a difference between what the two doctors were doing.
Spasticity and Numbness
by KHADAG RAJ
(Dubai)
Question: After almost 6 month of stroke, I started feeling spasticity on my left rib cage and other parts and tingling sensation started increasing my left palm towards left elbow/hand. I'm having difficulty in breathing and heaviness on left side and feeling of suffocation. I got ECG/ X RAYS/ 3T TEST for heart issue but everything was fine.
Now just done one MRI and again and waiting for report day after tomorrow.
Answer: If all your tests come back okay, you might consider looking into tightness/spasms in the muscles between the ribs (the intercostal muscles). Your symptoms sound similar to what happens to multiple sclerosis patients that have MS Hug if you want to look it up. Stroke can cause spasticity and tightness in various muscles, so maybe the muscles between your ribs are being affected. Some solutions might be massage, therapy to address ribcage tightness, yoga/meditation, or discussing medication options with your doctor that may help relax the muscles if that is what is causing your symptoms.
Treatment Tips from Others
To see tips from other survivors and caregivers about their treatment recommendations, click here.
Get Our Stroke Rehab Guide

Our stroke rehab guide is designed specifically for patients and caregivers. It's in pdf format and can be immediately downloaded. It includes about
- Stroke Definition & Causes
- Stroke Treatment
- Rehabilitation Information for Physical, Occupational and Speech Therapy
- Exercise pictures
- Q&A from patients and caregivers
- Adaptive Equipment & Techniques
- How to Prevent Another Stroke & More!
Medical Disclaimer: All information on this website is for informational purposes only. This website does not provide medical advice or treatment. Always seek the advice of your physician or other healthcare provider before undertaking a new healthcare or exercise regimen. Never disregard professional medical advice or delay seeking medical treatment because of something you have read on this website. See the disclaimer page for full information.
- Home
- Stroke Questions
- Spasticity and Numbness